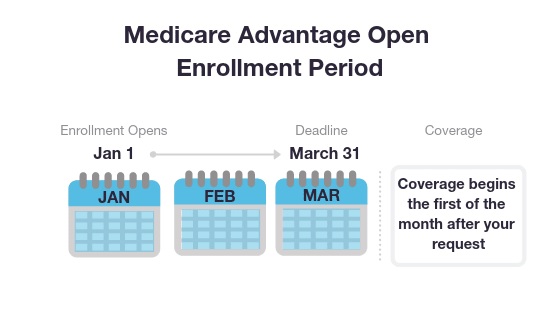
Medicare Advantage Open Enrollment Period: January 1 – March 31
If you're already enrolled in a Part C plan, you may switch Medicare Advantage plans or drop your Medicare Advantage plan and return to Original Medicare during this period which lasts from January 1 to March 31 every year.
If you return to your Original Medicare during this period, you'll also be able to join a Medicare prescription drug plan, Part D.
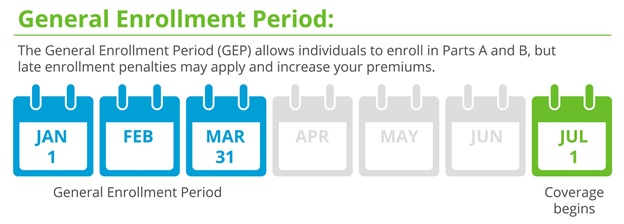
General Enrollment Period: January 1 – March 31
The General Enrollment Period is for individuals that did not enroll in Parts A or B when they were first eligible or if they lost their part B due to non-payment of their Part B premiums. You can sign up between January 1–March 31 each year. Your coverage starts July 1. You might pay a monthly late enrollment penalty if you don’t qualify for a Special Enrollment Period.
Medicare Special Enrollment Periods (SEP)
You may potentially be granted a Medicare Special Enrollment Period (SEP) depending on your specific circumstances. You could qualify for a Medicare SEP at any time of the year.
Metro Valley Insurance can help you find out if you qualify for a Medicare Special Enrollment Period (SEP).